Can a heartbeat or two really cause this much trouble?
Atrial fibrillation kills three times as many people as car accidents each year in the Western World. The cost per person is greater than that for cardiovascular disease and osteoarthritis, and it is twice that of obesity.
It affects 1% of the population and over 15% of individuals over 80 years of age.
The cost to society is in the billions of dollars.
The cost to individuals is immeasurable.
Cardiac epidemic
Don’t bury your head in the sand over this. An ageing population and our western lifestyle are ensuring that the prevalence of atrial fibrillation is increasing at such a rate that it is predicted to be the next cardiac epidemic.
Atrial fibrillation explained
It is very likely that you or someone you love is one of the 30 million people worldwide who has the ‘irregularly irregular’ heartbeat of atrial fibrillation. Or, it is possible that you may be among the people who do not realise they have this highly unpredictable condition, the personal impact of which can range from inconvenience to blackout, heart failure or stroke.
My book, Atrial Fibrillation Explained, is the ULTIMATE GUIDE TO ATRIAL FIBRILLATION
I unpack the intricacies of the 'irregularly irregular' heartbeat in my book, Atrial Fibrillation Explained.
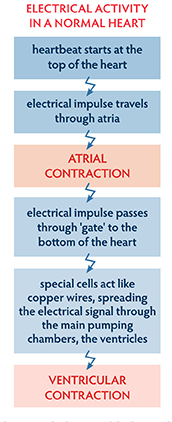
AF is a heart rhythm disorder that arises within the electrical system of the heart. Basically, the person has an irregular heartbeat, commonly described as abnormal, sudden, rapid, irregular, or chaotic, that affects the pumping capacity of the heart.
The heart can be likened to a car engine with compression chambers and valves, an electrical system and a set of fuel lines.
The car has pistons and valves as part of its power-generating engine block while the heart has as its pistons the compression chambers, the main one being the ventricle, and valves which stop the blood flowing back from where it came.
The car engine also requires a fuel line to supply the engine block. In the human heart, the fuel lines are the coronary arteries that literally provide the lifeblood to the engine block, the muscle of the heart. As a car engine has an electrical timing system, so does the heart. The electrical system in the heart ensures synchronicity and co-ordinated contraction throughout the heart. It also allows a mechanism for acceleration and deceleration. AF arises is this electrical system.
Healthy heart
A healthy heart is a highly efficient pump coordinated by its electrical system. The chambers of the heart, atria (top) and ventricles (bottom), work together, alternately contracting and relaxing, to pump blood through the lungs and the heart and into the body. The heartbeat is triggered by electrical impulses. The heart pumps 3 to 4 litres of blood every minute, with a healthy heart rate between 50 and 100 bpm. In a healthy heart, this pumping is synchronous, coordinated, smooth.
Breakdown
When the synchronicity breaks down, arrhythmia occurs. One of the most common forms of heart arrhythmia is atrial fibrillation, which has become one of the major causes of:
- stroke
- heart failure
- sudden death, and
- cardiovascular disease worldwide
AF results in chaotic, or irregular, electrical activity which causes the atria not to contract properly. Instead, they shake, vibrate, tremor; they fibrillate. Long-term atrial fibrillation can damage the structure of the heart and sometimes existing heart problems can trigger atrial fibrillation.
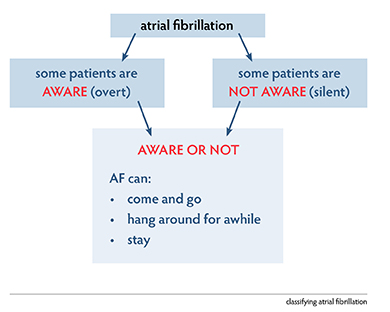
There are two types of AF:
- that which the patient feels, called overt, or symptomatic, atrial fibrillation, symptoms can include:
- palpitations in the chest
- an irregularity or a fluttering which they can describe quite clearly
- shortness of breath on exertion
- noticeable decrease in exercise capacity
- low blood pressure
- some patients may present after a collapse; and
- the AF of which the patient is not aware, called silent, or asymptomatic, atrial fibrillation
- because the person does not feel it at all, it is discovered as an incidental finding.
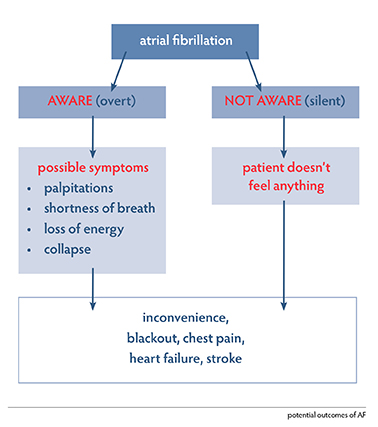
3% of the population over 75 years of age will have AF and not be aware of having the condition
AF is also classified in terms of the time the patient is in the abnormal rhythm:
- paroxysmal (comes and goes),
- persistent (stays longer than 7 days) or
- permanent (present for longer than a year).
Remainder-of-life management
Despite it being so widespread, AF does not allow a one-treatment-for-all approach nor can it be cured, so you could have it for a long time. Atrial fibrillation is associated with a poorer quality of life as sufferers’ symptoms include:
- lethargy
- palpitations
- breathlessness
- chest tightness
- sleeping difficulties
- psychosocial distress.
If it comes on suddenly, there is also understandable fear and anxiety.
In managing atrial fibrillation, medical carers look to the efficiency of the heart as a pump, its rate and its rhythm, and stroke mitigation, as the significant concerns. The condition, regardless of its type and time in arrhythmia, can be managed with:
- medication
- lifestyle adjustments, and sometimes
- procedural intervention.
Remember: currently, AF cannot be cured.
In my book, Atrial Fibrillation Explained, I discuss the tricks of living with this incurable problem.
a word from Joe, patient, Hobart
When diagnosed, I was unaware that I had atrial fibrillation. I had been aware of ‘something’, but thought it was due to tension and pressure of work. After being referred by my GP, we discovered that I was close to having a heart attack. This was something of a surprise as when I was younger, I had been fit, ate a healthy diet and there was no family history of heart problems. After discovering the presence of atrial fibrillation, I soon began recognising the signs of an episode.
Mostly, it occurred in the early hours of the morning when I was asleep. It would wake me up. I would feel uncomfortable, with the tightness in my neck, my chest pounding and sometimes with an ache in my arm. My brain felt as if it was scrambled; it was hard to think logically. When such an episode occurred, I would ensure that I was warm and sit in a chair next to the phone until it passed. It was quite scary, and, at times, I thought it might be the end. I have had an ablation which worked for a time. I also tried different medications and concentrations.
Now the condition has settled down. Even so, I often wonder when it will come back. In the meantime, I am so thankful that with patience and trying different approaches, I am currently in a good position.
The heart is still pumping isn’t it? So, what is the problem?
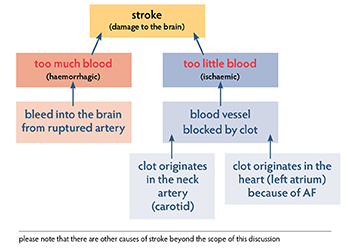
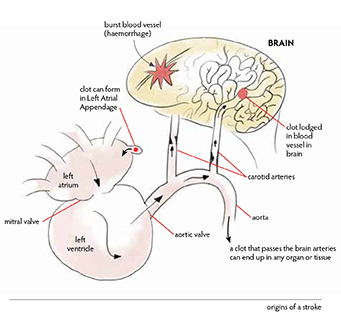
AF puts people at higher risk of stroke. This is when a blood clot goes from the heart to the brain. This neurological problem can result in localised weakness, difficulty with speech, difficulty with vision and even lead to death.
One-quarter to one-third of strokes are due to clots formed in the heart in someone with AF. The clot breaks off and causes a blockage in the blood flow to the brain.
This risk can be substantially reduced with modern therapy. To receive this benefit, people need to know that they have AF and then what they should do.
AF requires a team effort involving the people who suffer from AF and their families, their doctors and other health professionals. There can be a number of options for treatment and people need to work with their doctors to agree on what is best for them.
In my book, Atrial Fibrillation Explained, I add lots of useful and interesting additional pieces of information to add to an already revealing picture.
Stroke is a devastating occurrence. In the simplest terms, stroke is an interruption of the blood flow to the brain, an organ which needs a good supply of blood at all times. If there is any change in that flow, the tissue of the brain can be damaged. Damage to the tissue of the brain from a change in, or interruption to, the blood flow is a stroke.
There are two main ways a stroke can occur, resulting in an haemorrhagic stroke (when a blood vessel supplying an area in the brain bursts or ruptures, it bleeds into that area causing damage)
an ischaemic stroke (when a clot blocks the artery, leading to a lack of blood flow. There are two main locations where this kind of clot may form. The most common is within the large blood vessels in the neck, the carotid arteries. The other major clot source is the heart as a consequence of AF.)
When the left atrium is not contracting properly, blood can pool within a recess in the left atrium, the left atrial appendage. If blood pools in the appendage, a clot can form and subsequently dislodge. It can float into the left atrium, sweep through the mitral valve into the left ventricle. The ventricle will expel blood, including the clot, into the aorta. It will then come to the arch of the aorta where there is an opportunity for that clot to travel to the brain via either of the carotid arteries, and subsequently become lodged in a blood vessel within the brain, leading to an ischaemic stroke.
You may not know you have it, but I can soon tell, and I explain the fascinating detail of how in my book, Atrial Fibrillation Explained.
Diagnosis
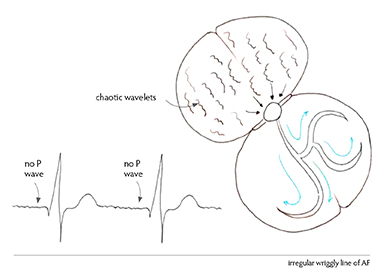
Central to diagnosing atrial fibrillation is monitoring the electrical activity of the heart. The traditional, simplest and most convenient way of determining that the heart rhythm is normal or otherwise is with an ECG, an electrocardiogram. This allows the electrical activity of the heart to be seen from different directions. Twelve electrodes monitor the electrical flow. The result is printed out or viewed on a screen.
The electrical activity in the atria is referred to as a P wave and it reflects atrial depolarisation. As the electrical impulses pass through the atrioventricular (AV) node and then on to the special distribution cells, a QRS complex is created, reflecting the depolarisation of the major muscle of the heart. The last part of the electrical heartbeat is the T wave and this is the return of normal repolarisation to the heart muscle, ready for the next beat.
So, in the normal heart, we see sinus rhythm, a beautiful synchronous atrial contraction followed by a beautiful synchronous ventricular contraction.
In atrial fibrillation, the atria lose their synchronicity; the beats become chaotic and irregular. The AV node, the gateway to the electrical stimulation of the bottom of the heart, is bombarded by chaotic electrical activity, producing a heartbeat that is referred to as ‘irregularly irregular’. The atria are not working, the ventricles are beating in an irregular way and, so, the pump can’t work properly.
Diagnostic thumbprint
In a normal ECG, a P wave is followed by a QRS and a T. In atrial fibrillation there is no P wave. Instead, an ECG trace baseline shows bumps and irregularities and an occasional QRS complex from depolarisation reaching the ventricle, occurring irregularly and unpredictably. This is our diagnostic thumbprint. Until we obtain a clear electrical tracing, we can’t be sure of the rhythm.
Other options
An ECG which monitors the heart for just a few minutes might not be long enough to establish if atrial fibrillation is present. If someone seems to be going in and out of atrial fibrillation with some regularity, then the medical practitioner has some options:
- to ask the patient to wear a Holter monitor for several days. The result is not as detailed as from a 12-lead ECG, but it gives good information over a 24-hour, 48-hour or three-to-five-day period;
- implant a small monitoring device. In some patients, there can be the suspicion that AF is occurring, but not frequently. If the cardiologist believes that the importance of making a diagnosis is high enough, then a very small device called a loop recorder may be implanted under the skin above the heart. This remains in place for up to three years;
- take a person’s pulse.
AF can also be discovered incidentally, such as during monitoring in association with surgery or the patient being in a high dependency unit, or during the routine interrogation of a pacemaker. Regardless of the method by which the trace is achieved, lack of a P wave on an ECG or its equivalent gives the diagnosis of atrial fibrillation.
case study – Peter
accidental finding

Peter was a 65-year-old man when his atrial fibrillation was found incidentally. A week or so before I met him, late in 2017, Peter was undergoing a routine colonoscopy, a test to look in his lower bowel. The anaesthetist who was looking after him found his pulse to be ‘irregularly irregular’ with a controlled rate. An ECG and subsequent monitoring confirmed that Peter was in atrial fibrillation, although he had had no clue as to his situation as he had experienced no symptoms. This is not entirely uncommon. A number of people do walk around with silent or asymptomatic fibrillation.
When I spoke with Peter, it turned out that he had seen his GP about three months earlier. His blood pressure and pulse, which were checked at the time, were said to be okay. This suggests that he had gone into fibrillation in that intervening period. Peter’s general health also included some hypertension for which he was on therapy and central adiposity or weight around the belly. This can be a marker of pre-diabetes and is worth keeping in mind. He did not exercise much.
When we looked at Peter’s risk of a stroke on the CHA₂DS₂-VASc score (a clinical predictor for estimating the risk of stroke in patients with atrial fibrillation) he had a score of two: one for age and one for hypertension. I would have added an extra score for pre-diabetes. However, with a score of two, his risk of stroke was considered mild to moderate with the recommendation that he should be on full anticoagulation.
When I spoke with Peter, it turned out that he had seen his GP about three months earlier. His blood pressure and pulse, which were checked at the time, were said to be okay. This suggests that he had gone into fibrillation in that intervening period. Peter’s general health also included some hypertension for which he was on therapy and central adiposity or weight around the belly. This can be a marker of pre-diabetes and is worth keeping in mind. He did not exercise much.
We also had other information available. A 24-hour heart rate monitor showed that in the asymptomatic state, on average, Peter’s heartbeat in atrial fibrillation was nearly 100 beats a minute, going as high as 180 beats a minute at times of exertion. For someone in his mid-60s, that’s a very fast heartbeat and I was quite surprised that he was asymptomatic. An ultrasound of his heart showed that the structure and function of Peter’s heart were relatively normal, although his atria were mildly to moderately dilated.
As a result of the CHA₂DS₂-VASc score, I started Peter on full anticoagulation. I also included in the therapy a drug to try to slow the heartbeat down. A heart that’s revving so quickly simply does not fill properly and therefore doesn’t pump properly, and so patients almost invariably describe some shortness of breath. This should give him more puff as the heart pumps better.
Another consideration for Peter was whether or not we should attempt to restore sinus rhythm. On occasions, we can be caught between trying to restore normal rhythm and leaving people in atrial fibrillation. The lack of symptoms, as in the case of Peter, can suggest an approach that simply controls the heart rate. However, in this particular situation, the patient is relatively young. My observation over the years, and there is some research coming through to support this, is that if we restore sinus rhythm, we may have a positive effect on any morphological, or structural, change the heart could undergo. What I mean by that is, if we leave people in atrial fibrillation for many years, we see changes in the heart as a consequence of that atrial fibrillation. The most notable alteration is that the atria dilate or enlarge. Another observation, and I have a number of cases in which this has occurred, is the atrioventricular ring that connects the atrium to the ventricle also dilates as the atria dilate. If the AV ring dilates, then the fixtures for the alves that it holds, particularly for the tricuspid valve which is on the right side of the heart, can be stretched.
As it stretches, the cusps of that tricuspid valve do not come together as well as they should. So, although I haven’t yet attempted to restore sinus rhythm in Peter, it’s a serious consideration so that the structure ofhis heart can be maintained in its best condition for as long as possible.
Regardless of whether I return him to sinus rhythm or not, Peter will be on anticoagulation for the remainder of his life. The CHA₂DS₂-VASc score is high enough, and with his being completely unaware of symptoms, I wouldn’t begin to rely on him to tell me when he’s in and out of the rhythm.
Who suffers from AF?
Men suffer from atrial fibrillation as do women. More men develop the disease; however, women, when they suffer from the condition, run a higher risk of complications, including death. Although there is an increasing incidence of the condition as people age, young people, even as young as in their teens, can suffer from it, although it is uncommon.
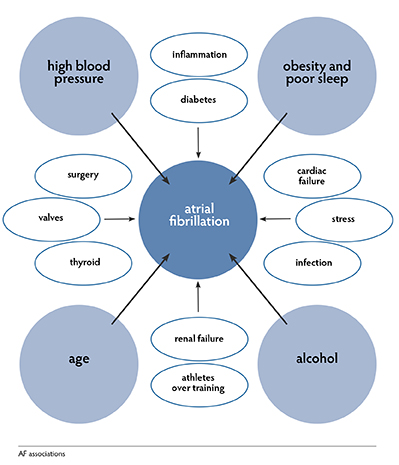
Associations
Atrial fibrillation associations are found within the heart structure as well as externally. In coming to a better understanding of atrial fibrillation, it is valuable to understand AF associations. Associations are the factors that lend weight to the possibility of AF being present, but they are not the mechanisms that give rise to the actual problem.
Within the heart
- high blood pressure
- micro scarring
- general wear and tear
- problems with the valves
- abnormality of the muscle
- cardiac failure (including congenital heart problems)
Outside the heart
- obesity
- obstructive sleep apnoea
- diabetes
- chronic renal disease
- external toss toxins such as alcohol
- pulmonary thrombi embolism
- genetic disposition
- thyroid problems
- infections and inflammation
- emotional stress
- surgery
- endurance training
The big three associations are:
- obesity
- high blood pressure
- alcohol
Each of these can be modified by the patient. The one that can’t be controlled is age.
These associations all cause strain on the body and particularly the heart. AF can be a common final pathway of stress within the body. Being aware of problems that can be associated with atrial fibrillation is a really important first step towards avoidance or management of the condition.
case study – KAREN
post-operative
Karen was a 75-year-old woman when I first met her. She was generally fit, well and active. She had had surgery for a colorectal problem. In the post-operative period, she developed AF. I was called and over the phone I recommended some digoxin to slow the heart rate down and also some metoprolol to slow down the heart rate with the potential of reverting the atrial fibrillation back into sinus rhythm.
Before I saw her several hours later, clinically, she had returned to sinus rhythm. On speaking with her, it became clear that she had had episodes of palpitation in the past. I was comfortable in letting her go home on some regular metoprolol, hopefully to keep her out of trouble. I also put her on low-dose aspirin because she had just had surgery and I didn’t want the risk of bleeding after the surgical procedure. I looked to re-view her in my rooms several weeks after her surgery and at that stage I also hoped to review her echocardiogram and Holter monitor testing.
The results of the echocardiogram showed that she had a dilated left atrium. This suggested that there was a reasonable chance she would have future recurrences of atrial fibrillation. That supported her reports of having had palpitations before the documented post-operative episode. The Holter monitor, which recorded the electrical activity of her heart over 24 hours, showed multiple episodes of short bursts of atrial ectopy, or extra beats arising from the atria. These can be a trigger for atrial fibrillation and for Karen they were occurring while she was on metoprolol. I was happy to keep her on metoprolol to try to dampen down the likelihood of the occurrence of palpitation.
She reported feeling really well and tolerated the metoprolol without issue. However, I thought there was a reasonable chance that, as time progressed, her AF threshold would reduce and, therefore, her likelihood of recurrence would increase. So, I swapped the aspirin to a NOAC to keep the blood thin. Karen was happy and she was well. We planned to touch base in six months to ensure that everything was travelling smoothly. So, Karen’s post-operative atrial fibrillation was managed in the longer term on a beta-blocker (metoprolol) and anticoagulation, with regular follow-up planned.
Are all palpitations AF?
The simple answer is “No”.
Rapid and irregular
- AF is a possibility
- atrial ectopic beat
- ventricular ectopic beat
Rapid and regular
- atrial flutter
- supraventricular tachycardia
- ventricular tachycardia (not common but high-risk rhythm)
- ventricular fibrillation (not felt, causes sudden death from cardiac failure)
Treatment information
Once atrial fibrillation has been diagnosed and the relevant associated information for the patient has been gathered, there are three areas of focus for AF management:
- heart rate
- risk of stroke
- if the patient should be returned to normal rhythm.
One also needs to understand risk-benefit in relation to the patient’s condition.
Heart rate
Because of the chaotic beat within the atria, the heart is racing, often as fast as 150 and sometimes over 200 bpm, irregularly. This is very distressing to the person. At this rate, the heart doesn’t work, or fill, properly so the speed needs to be slowed.
Risk of stroke
Risk of stroke is of concern because, when the atria are not contracting properly, blood can pool, particularly in the left atrial appendage. Where it pools, a clot can form. Should this happen, the clot can find its way to the brain, leading to a catastrophic outcome, a stroke. To lower this risk, the blood needs to be ‘thinned’. As part of the management strategy, especially around anticoagulant therapy, we utilise the CHA₂DS₂-VASc score, a clinical predictor for estimating the risk of stroke in patients with AF. Then, to determine the risk of complications from bleeding, another score, HAS-BLED, is used.
Returning the heart to sinus rhythm
A number of factors come into play in the decision of whether or not an attempt should be made to bring the person’s heart back to normal, or sinus, rhythm.
Understanding risk-benefit of medication
There is no medication available that has zero risk, so it is essential that patients be clear about what any risk might be. However, risk needs to be put into the context of the benefit and benefit generally needs to be considered in the light of two different components:
- the symptomatic benefit (improving the way the patient feels) and
- the prognostic benefit (improving the long-term outcome).
DR DAVID O’DONNELL
Electrophysiologist and Cardiologist
Melbourne, Australia
from the Preface
This book provides an excellent introduction to atrial fibrillation and a comprehensive review of the management options available for AF.
The management of atrial fibrillation is complex and can be confusing. A number of different approaches and a number of different strategies are possible, depending on the specifics of the person with atrial fibrillation and the expertise and interest of the treating doctor. I think this book is an ideal resource for anyone diagnosed with atrial fibrillation or living with someone diagnosed with atrial fibrillation. Presenting to your treating cardiologist or electrophysiologist with a better understanding of atrial fibrillation will improve the doctor-patient experience and ensure that the best outcomes can be achieved.
Treatment
To slow the heart
- beta-blockers
- digoxin
- calcium channel blockers
- amiodarone
To thin the blood
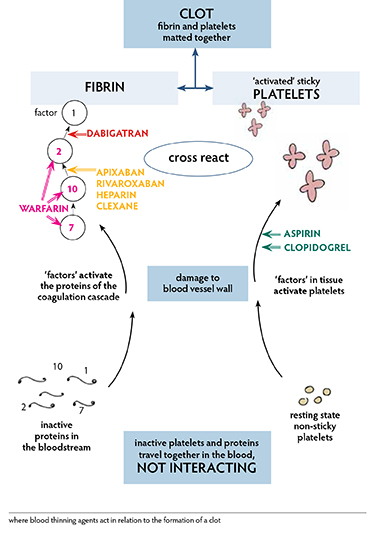
Acutely, heparin, clexane, NOACs (sometimes called DOACs which are new agents on the market, Direct or Novel Oral AntiCoagulants. These agents act directly on the coagulation cascade and each acts quickly. Most conveniently, these medications do not need regular blood tests to monitor their effect. NOACs include the drugs apixaban, dabigatran and rivaroxaban.)
Long-term, warfarin or NOACs.
To keep a heart in sinus rhythm
Although there is not cure for AF, some patients can be kept ion sinus rhythm for years. Returning a patient to sinus rhythm has symptomatic benefits; yet, surprisingly it does not reduce the risk of an adverse event in the long term. For those in whom sinus rhythm is not restored, over time, they become used to living with AF.
Sinus rhythm is restored by using drugs or electricity. Treatment needs to look at rhythm control as well as anticoagulation and is dependent on:
- the timing of presentation in relation to the episode
- the structure of the patient’s heart
- the general medical condition of the patient.
Factors contributing to the decision to try to keep a patient in normal rhythm include:
- the unacceptable nature of the symptoms
- the age of the person.
Keeping a person in sinus rhythm is achieved by:
- addressing reversible factors such as weight, obstructive sleep apnoea, alcohol consumption, high blood pressure, thyroid function and control of other diseases
- medication
- EP ablation
In my book, Atrial Fibrillation Explained, I go into a lot of detail about the drugs and surgical procedures associated with the on-going treatment of AF
PROF. GARRY JENNINGS AO
Cardiologist and Executive Director
Sydney Health Partners
Sydney, Australia
from the Foreword
We know from surveys that knowledge about heart disease in the general community is low. This book is one of a series written by Dr Warrick Bishop to help remedy the situation. It is a personal account from a busy cardiologist trying to span the gap between what doctors know about AF and what those with AF and their loved ones need to know. It is informed by the latest guidelines but also includes personal anecdotes and the stories of real people who have experienced AF.
A WORD FROM THE AUTHOR
Hi, I’m Dr. Warrick Bishop, and thank you for being interested in my latest book, ATRIAL FIBRILLATION EXPLAINED, the ultimate guide to this troublesome ailment.
I have written this book because this very common condition, especially in older people, warrants good information and good education so that patients can be engaged in their own best management.
Throughout the book, I explain:
- what the condition is
- how we diagnose it
- how we treat and manage it and
- how that impacts on the patient.
I scrutinise atrial fibrillation in a way that allows patients and medical practitioners to understand the best way to look after the condition in personal sets of circumstances. While this book provides interesting and useful details, it also poses questions, hopefully resulting in some significant and revealing discussions between you, the individual, and your medical care providers. And don’t forget to include your family.
My aim is to minimise the symptoms as safely as possible and to maximise your prognosis. I want you to “live as well as possible, for as long as possible”.
MY BOOK, ATRIAL FIBRILLATION EXPLAINED, IS A MUST READ
“This is the best patient-focused atrial fibrillation book that I have read.” - DR DAVID O’DONNELL, electrophysiologist and cardiologist, Melbourne, Australia (preface)
Must-Read For:
- sufferers
- those who care for them
- medical practitioners and
- anyone planning to leave into a healthy, old age.
Having a better understanding of AF as a disease and learning about its treatment will open up meaningful conversations between patients and their medical practitioners as well as their families and friends, leading to greater insights into the best way to look after the condition and to live with it in personal sets of circumstances.
Understandably, there are a lot of practical questions associated with atrial fibrillation. Some include:
- What is the best way to reverse the effects of warfarin and NOAC?
- Should I swap warfarin for NOACs?
- Do I need a pacemaker?
- Do I need a stress test or angiogram?
- Can I be screened for AF?
- Do I need to store AF drugs in a particular way?
- How often do I need testing or to see my cardiologist?
- What effect does caffeine have in relation to AF?
- Can I exercise safely?
- What if I need to have surgery?
- Can I stop the medications if I feel well?
And of course, there is always the question of how do we deal with complicated situations? What if we are dealing with a patient who:
- is elderly, frail and liable to fall?
- has need of a stent a narrow artery?
- has cardiac failure?
- has severe renal failure?
- has other complications such as AV malformations or a cerebral bleed?
In Atrial Fibrillation Explained, the ultimate guide to AF, I answer these questions, and more, in detail.
- The book is a resource specifically written to help patients, nurses, doctors and families who want more information about this common and challenging condition.
- The information is based on current guidelines and is written using simple language.
- The book offers precise yet understandable detail with the help of plenty of patient histories to help explain this complex and frequently encountered condition.
In my book, Atrial Fibrillation Explained, there are lots of case studies, graphics, tables and cartoons to help you understand the more technical AF information
I love this story. Within the setting of routinely looking to anticoagulate patients to reduce the risk of clot formation in the heart and a subsequent stroke, anticoagulation is a really important component of management, and yet … I have had elderly patients who remain active and are not frail. I had one patient who regularly went into the bush where he used a chainsaw. He had been a blogger all his life and that was not going to change. So, we took this into account when deciding on his care:
- the man being 80+ years of age
- in the bush with a chainsaw and other sharp pieces of equipment, and
- a long, long way from help.
He still went on anticoagulation, but not before a detailed discussion which led him to understand the pros and cons of his situation.
from the Preface:
"Warrick has an unique ability to demystify complex medical issues. His style is factually accurate and scientifically complete, yet free of the medical jargon typically used by many in our profession. I have frequently recommended his previous book, Have You Planned Your Heart Attack?"
DR DAVID O’DONNELL Electrophysiologist and Cardiologist, Melbourne, Australia
In summary
Atrial fibrillation is a common medical condition, the symptoms of which can come and go, come and hang around for a while, or come and stay. In any scenario, once you have it, you have it for the remainder of your life. It cannot be cured, only managed.
You can reduce your own AF risk by ensuring your blood pressure is well managed over your lifetime, maintaining a healthy weight which will also reduce your risk of obstructive sleep apnoea, and refraining from excess consumption of alcohol.
Many people feel the symptoms; many do not know they have it. For some, the symptoms can be debilitating while for others, they are an inconvenience. Successful treatment is highly personalised and can take patience and perseverance to establish and maintain.
Symptoms aside, the biggest concern regarding atrial fibrillation is risk of stroke, a catastrophic consequence that will occur on average at a rate of five percent a year in an untreated group of atrial fibrillation sufferers.;
People with atrial fibrillation need blood thinners, but people with AF also need operations and people with AF have accidents. Atrial fibrillation is a bleeding problem for those on blood thinners and a clotting problem for those not on thinners.
The risk of stroke must be balanced with the risk of bleeding, and both risks increase with age and the complexity of other medical conditions being suffered by the patient.
Development of the NOACs has been one of the single most significant advances in the management of atrial fibrillation in recent years as their ease of use provides much more convenient anticoagulation without the fluctuating dose adjustments and repeated blood tests needed with the use of warfarin, with the same or better efficacy.
Daily, I see the suffering associated with heart disease and our specific interest here, atrial fibrillation. Simple lifestyle maintenance can reduce your risks substantially. However, if you already have atrial fibrillation, attention to good management with the help of your medical practitioner can considerably improve your symptoms and so your daily living, for some, even providing lengthy symptom-free living. My deep desire is to provide you with information that can help you to be involved in your own destiny, to give yourself the best chance for a healthy life. For a much greater depth of detail, please purchase the book, Atrial Fibrillation Explained, and subscribe to my Healthy Heart Network.
I wish you good health and a long and happy life.